The Impact of Bariatric Surgery on the Psychiatric Morbidity of Patients with Morbid Obesity
Saenz-Herrero M, Lopez-Ibor JJ, Cabranes JA, Gonzalez-Pinto A
DOI10.21767/2471-8203.100007
Sáenz-Herrero M*, Marta Zubia, Nuria Nuñez López-Ibor JJ1, Cabranes JA1, González-Pinto A2
1Institute of Psychiatry and Mental Health, Hospital Clínico San Carlos, C/ Prof. Martín Lagos s/n Madrid 28040-Madrid (Spain)
2Alava University Hospital. Basque Country University, Vitoria, Spain
- *Corresponding Author:
- > Margarita Sáenz, MD, PhD
- Associate Professor. Psychiatry Department.
Institute of Psychiatry and Mental Health. Hospital Clínico San Carlos
Madrid, Spain. Alava University Hospital. Vitoria. Spain. UPV-EHU. CIBERSAM
Tel: 0034650484939
E-mail: msaenzherrero@yahoo.es
Received Date: September 28, 2015; Accepted Date: October 30, 2015; Published Date: November 04, 2015
Citation: Margarita S, Zubia M,Nuñez N,Ibor JJ,Cabranes JA,González-Pinto A (2015) The Impact of Bariatric Surgery on the Psychiatric Morbidity of Patients with Morbid Obesity. J Obes Eat Disord 1:7. doi: 10.4172/2471-8203.100007
Copyright: © 2016, Margarita S et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Morbid obesity (defined as a body mass index (BMI) >40) is a severe and increasingly prevalent condition in developed countries. On top of medical dysfunctions a large proportion of these patients also suffer from psychosocial dysfunctions and psychiatric disorders. Prior to bariatric surgery a substantial percentage of patients suffer from binge eating disorder or binge eating symptoms. Surgery is carried out not only to reduce short term morbidity and mortality in patients with morbid obesity but it also gives a chance for a long-term weight loss. To achieve this goal many patients need some kind of psychiatric intervention.
Objective: The principal aim of this study is to evaluate the impact of bariatric surgery on psychiatric disorders and psychological dysfunctions of patients with morbid obesity over the course of a year following surgery. Special consideration is given to the presence of psychiatric comorbidity, eating disorders, body image dissatisfaction and self-esteem.
Design: Longitudinal, psychiatric intervention previous and one year after surgery.
Results: The mean age of the patients was 41.7 years (SD=2.4) The mean weight was 121.8 kg (22.5) which corresponds to a mean BMI of 45.7 (7.7). The sex distribution is 20% male and 80% female patients. Psychiatric disorders (ICD-10 criteria), were present in 32.5 %. Among them eating disorders were the most prevalent (38.5%). Following bariatric surgery there was a significant improvement in eating disorders and eating symptoms (according to the Eating Disorders Inventory and the Bulimic Test of Edimburgh) and in body image satisfaction (measured by BSQ) and self steem (Rosemberg). A multiple regression analysis of clinical factors associated to weight loss showed that 40% of it is determined by the decrease of bulimic symptoms detected by the BITE-symptoms.
Conclusion: Morbid obesity is a risk population for psychiatric disorders and psychological dysfunctions. Bariatric Surgery reduces over one year the severity of this morbidity. The impact of increased self-esteem through the increase of body image satisfaction and of the increase in control over food intake seems to be the major factor in these changes.
Keywords
Morbid obesity; Bariatric surgery; Psychiatric comorbidity; Eating disorders; Impulsivity
Introduction
Obesity is a chronic and a serious public health problem in Western countries and in many non-Western countries. The literature has presented well-documented links between obesity and increased mortality and medical morbidity [1,2]. Morbid obesity (defined as a BMI>40) is a serious and increasing prevalent condition in developed countries. On top of medical disorders associated to, a large proportion of these patients also suffer psychiatric disorders and psychosocial disfunctions. Bariatric surgery is carried out to reduce morbidity and mortality associated to the high BMI, with the hope that the loss of weight can be mantained for long time [3]. The adverse effects of obesity are not only medical. In Western countries negative attitudes toward obesity are highly prevalent in society. At least 30-50% morbid obese patient’s prior surgeries meet criteria for binge eating disorder or suffer from binge eating symptoms [4]. Most investigations found higher levels of eating behaviour disturbances related and general psychiatric symptomatology in obese patients with binge eating disorders than those without binge eating [5-7]. Binge eaters have more psychiatric comorbidity (personality, anxiety and mood disorders) [8,9], or symptoms (distortion of body image, depression, high impulsivity) and more vulnerability to negative comments about shape, weight and eating [10]. Severe obesity is associated to more vulnerability for mood disorders [8-11]. Candidates for surgical intervention are more impulsive, irritable and anxious that obese patients treated conventionally [12]. These differences between these two groups are in line with other studies that have shown a significant heterogeneity in the obese population. For instance, those seeking treatment report higher levels of distress compared to those not seeking treatment [13,14] and patients who prefer more drastic weight reduction methods, such as surgery or appetite supressants, differ on psychological variables from those who prefer conventional treatments such as diet [15-17]. Although body image distortion is a major diagnostic component in eating disorders there is no uniform description of its relation to obesity [18]. Furthermore findings about body image distortion in obese patients are controversial, with some studies showing overestimation, others underestimation, and others no difference when compared with controls [18-20]. There are some suggestions that body image improves following weight loss [21] but more studies are needed to ratify these findings. Sex has been found to contribute to differences in body perception and body dissatisfaction. There is a tendency for obese and nonobese women to overestimate body size and to report more dissatisfaction than obese and non-obese males [22]. However the literature lacks studies comparing male and female’s obese subjects [23].
Methods
Participants and Procedure
All the subjects in the study (n=31) were recruited from surgical candidates before and one year after surgical intervention (Treat consisted on gastric banding, vertical banded gastroplasty or gastric by-pass)
Informed consent for the present study was obtained from all participants. The age of participants was from 18 to 65 years. Patients were excluded if they had a history of use or abuse of drugs and alcohol, schizophrenia or psychotic disorders, and severe bulimia nervosa. The assessment was completed in two sessions before and one year after surgery, lasting approximately 1 hour each. All tests were administered individually by the same psychiatrist.
Measures
A semi-structured clinical interview developed for this study was carried before and one year after surgery. It included history of dieting, history of obesity, clinical variables including weight and height. Body mass index was calculated (BMI=kg/m2) Subjects completed the following self-report measures prior and up to one year after bariatric surgery:
The body image dissatisfaction was evaluated with the Body Shape Questionnaire [19], which is a 34 item instrument that uses a 6-point Likert scale ranging from 1 (never) to 6 (always) to measure affective, cognitive, and behavioral dimensions of the attitudinal body image construct. Higher scores indicates greater body image distortion.
Eating disturbances were assessed with the Eating Disorders Inventory [24]. The EDI is a 64-item, self-report measure of eating behavior and thought patterns. It has eight subscales: drive for thinness, bulimia, body dissatisfaction, ineffectiveness, perfectionism, interpersonal distrust, interoceptive awareness, and maturity fears. The subscales have shown adequate internal consistency coefficients and have been well validated.
Bulimic symptoms were assessed by the Bulimic Investigatory Test, Edinburgh [25], which has two subscales: BITE-symptom and BITE-severity. The 33-item questionnaire was developed to assess bulimic attitudes and behaviors. The BITE has strong reliability and validity.
Depressive Mood was evaluated with the Beck Depression Inventory (BDI). This is a 21-item questionnaire where subjects rate the extent to which they experience cognitive, affective, and somatic symptoms of depression. There is much support for its reliability and validity as a measure of dysphoria in non-clinical and clinical populations [26].
Anxiety was assessed with the Hamilton Rating Scale (HARS)[27]. This is a 14-item questionnaire which was developed to assess physical, psychological and behavioral aspects of anxiety in the three days previous to the assessment.
Self-steem was assessed with the Rosemberg self-esteem scale [28], a 10-item measure of self-esteem that uses a 4-point scale ranging from 1 (strongly agree) to 4 (strongly disagree).
Statistical Analysis
The Student’s t-test or ANOVA were used to compare continuous variables expressed as means and standard deviation (SD) while categorical variables were compared using the chi-squared test. The Student’s paired t-test was used to compare continuous clinical variables (expressed as means and standard deviation (SD). Multiple regression analysis was performed to try to explain the weight loss (BMI difference). Variables shown to significantly influence by univariate analysis were included in a multivariate analysis. Adjusted parameter and their 95 percent confidence intervals (95% CI) were calculated. The null hypothesis was rejected in each statistical test when p<0.05. Analysis was performed using windows SPSS version 12.0 software.
Results
The mean age of patients was 41.7 years (12.4). The mean weight was 121.8 kg (22.5) which corresponds to a mean BMI 45.7 kg/m2 (7.7) kg/m2. 20% of the patients were male and 80% female. 32.5% of the sample fulfilled ICD-10 criteria for a mental disorder [29], and of them 38.5% of an eating disorder (11.8% of the total). The results of the weight changes (Tables 1 and 2), shows sociodemographic characteristics of the sample and Table 3 shows the changes in the psychological variables studied.
| PREmean (SD) | POSTSURGERY mean (SD) | Diferencia(CI 95%) | p | |
|---|---|---|---|---|
| Weight | 123.75 (25.02) | 90.23 (19.82) | -33.51 (-39.83; -27.21) | <0.001 |
| BMI | 46.37 (8.93) | 33.49 (7.80) | -12.89 (-15.17; -10.60) | <0.001 |
Table 1: Weight Changes following Bariatric Surgery.
| N=31 % (N) | ||
|---|---|---|
| SEX | Women Men |
80.6(25) 19.4(6) |
| NATIONALITY | Native Non-native |
93.5(29) 6.5 (2) |
| CIVIL STATUS | Single Married Divorced Widowed |
29.0 (9) 61.3 (19) 6.5 (2) 3.2 (1) |
| LIVING | Origin family Own Family Alone Others |
22.6 (7) 64.5 (20) 9.7 (3) 3.2 (1) |
| EDUCATIONAL LEVEL | Compulsory Secondary Graduate |
45.2 (14) 45.2 (14) 9.7 (3) |
| EMPLOYMENT | Active Unemployed Sick leave Housekeeper Student |
54.8 (17) 9.7 (3) 3.2 (1) 25.8 (8) 6.5 (2) |
Table 2 Sociodemographic Characteristics.
On the whole, the impact of surgery on the clinical variables was very important. There was a significant improvement in the presence of eating disorders and eating symptoms after bariatric surgery (measured by the Eating Disorders Inventory and the Bulimic Test of Edimburgh) body image dissatisfaction (measured by BSQ), self steem (measured by the Rosemberg Scale), anxiety (HADRS) and depressive symptoms (BDI) as shown in Table 3.
| EDI | PREmean (SD) | POSTmean (SD) | Difference(CI 95%) | p |
|---|---|---|---|---|
| Drive for thinness | 8.42 (5.43 ) | 6.16 (4.17) | -2.26 (-3.91;-0.60) | 0.009 |
| Bulimia | 2.64 (4.23 ) | 0.80 (2.41 ) | -1.83 (-3.37; -0.30) | 0.002 |
| Body Dissatisfaction | 18.6 (5.30 ) | 9.74 (7.30 ) | -8.87 (-11.84;-5.89) | <0.001 |
| Ineffectiveness | 4.16 (5.20 ) | 3.32 (5.55) | -0.83 (-2.33; 0.65) | 0.2 |
| Perfectionism | 3.96 (2.97 ) | 3.41 (2.94) | -0.54 (-2.22; 1.12) | 0.5 |
| Interpersonal Distrust | 3.06 (3.71) | 2.41 (3.66) | -0.64 (-1.94; 0.65) | 0.5 |
| Interoceptive Awareness | 5.48 (4.95 ) | 4.32 (4.82) | -1.16 (-2.96; 0.64) | 0.3 |
| Maturity Fears | 4.16 (4.05 ) | 4.09 (3.06) | -0.06 (-1.83; 1.70) | 0.1 |
| BITE | ||||
| Symptoms | 11.29 (6.63) | 5.83 (3.97) | -5.45 (-7.45; -3.44) | <0.001 |
| Severity | 4.29 (4.67) | 1.93 (2.80) | -2.35 (-3.88; -0.82 ) | 0.008 |
| ROSEMBERG | 30.16 (6.91) | 33.23 (4.90) | 3.06 (0.36; 5.77) | 0.003 |
| BDI | 14.03 (10.34) | 10.38 (9.37) | -3.65 (-6.5; -0.75) | 0.015 |
| HDRS | 11.58 (7.02) | 4.87 (6.41) | -6.70 (-10.07; -3.35) | <0.001 |
| BSQ | 106.81(39.12) | 85.22 (39.48) | -21.58 (-2.99;10.17) | 0.001 |
Table 3 Differences in psychometric variables before and after one year surgery.
Sex Differences
In general the surgery has a more significant impact on the psychosocial dysfunctions in women (Table 4) and this may be due to the fact that they have more psychopathology present prior to surgery.
| EDI | PREmean (SD) | POSTmean (SD) | Diference(CI 95%) | p |
|---|---|---|---|---|
| Drive for thinness | 9.60 (5.21) | 6.88 (4.33) | -2.72 (-4.68; -0.76) | 0.008 |
| Bulimia | 3.04 (4.59) | 1.00 (2.66) | -2.04 (-3.94;-0.14) | 0.16 |
| Body Dissatisfaction | 19.20 (4.88) | 11.36 (7.11) | -7.84 (-11.24; -0.14) | 0.65 |
| Ineffectiveness | 4.88 (5.47) | 4.00 (6.00) | -0.88 (-2.70;0.94) | <0.001 |
| Perfectionism | 4.12 (2.99) | 3.36 (2.97) | -0.76 (-2.65; 1.13) | 0.38 |
| Interpersonal Distrust | 3.32 (3.98) | 2.88 (3.94) | -0.44 (-2.01; 1.13) | 0.006 |
| Interoceptive Awareness | 6.48 (4.98) | 5.28 (4.90) | -1.20 (-3.44; 1.04) | 0.05 |
| Maturity Fears | 4.92 (4.13) | 4.16 (3.36) | -0.76 (-2.83; 1.31) | 0.59 |
| BITE | ||||
| Symptoms | 12.04 (7.00) | 6.32 (4.25) | -5.72 (-8.13; -3.31) | 0.004 |
| Severity | 4.80 (4.94) | 2.16 (3.06) | -2.64 (-4.48; -0.80) | 0.021 |
| ROSEMBERG | 29.20 (7.10) | 32.64 (4.94) | 3.44 (0.21; 6.66) | 0.34 |
| BDI | 16.35 (10.36) | 11.69 (10.09) | -4.65 (-8.18; -1.12) | <0.001 |
| HDRS | 13.21 (6.88) | 5.58 (7.00) | -7.63 (-11.77;-3.50) | 0.33 |
| BSQ | 114.68 (38.62) | 92.40 (39.29) | -22.28 (-35.71;-8.85) | <0.001 |
Table 4 Differences in clinical variables before and after 1 year postsurgery in 22 females patients with morbid obesity.
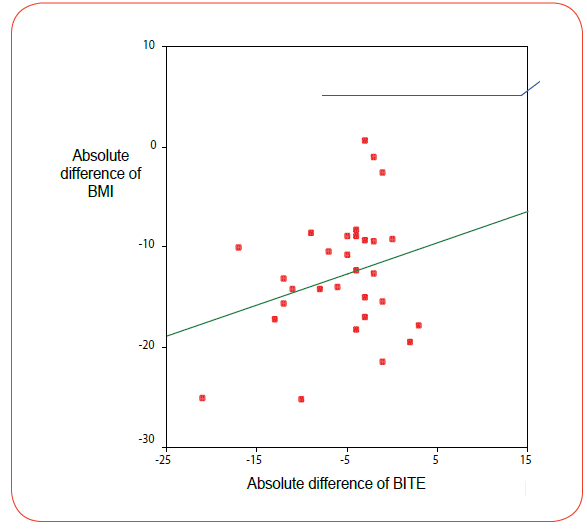
The main question is to know why and how surgery and the associated weight loss improves the psychiatric and psychological status of patients. In order to find an appropiate answer we conducted a multiple logistic regression analysis. The main finding of it is that 40% of the weight loss is determined by the decrease of bulimic symptoms detected by the BITE (Figure 1).
Discussion
Bariatric surgery has a high positive impact on the psychiatric morbidity and psychosocial functioning of patients with morbid obesity evaluated one year after surgery. At follow-up anxiety levels detected by HDRS and depressive symptomatology detected by BDI had improved among the patients after losing weight significantly. The higher levels of anxiety of obese patients before surgery predispose them to a lifestyle leading obesity [12]. The decreased levels of anxiety can be explained by the fact that severely obese generally suffer from comorbid conditions. Surgically induced weight loss improves functional health and is associated with a marked relief in dyspnoea, chest pain and asthma, and the weight reduction is associated with greater improvements in functional health [30-33]. Several authors have attributed the improvement of the psychiatric and psychological disturbances in morbid obesity to the impact of weight loss on body image [34]. Weight loss is associated with decreased distress [15,16].
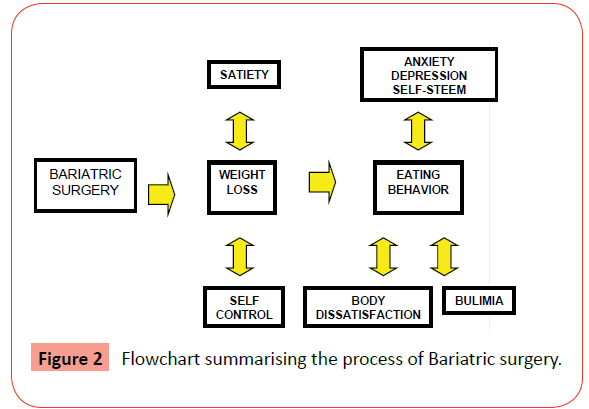
Our results show that another factor may be present, which the impact of surgery on the control of the impulse to eat and binge. BITE essentially measures impulsive behaviour related to food intake and the regression analysis shows a very high correlation of the weight loss and the reduction of the bulimic symptoms of the BITE. The effect of surgery on the eating behavior is indirect. Essentially bariatric surgery promoves its effects through a reduction of the volume of the stomach leading to an increase in satiety. This leads to an increase of the subjective sensation of self control over the eating behaviour and an improvement in the psychological self-image of the patient. As a consequence the satisfaction of the patient with him/her-self increases as he/she feels, more able to control food intake and the binges. This added to reduction of weight leads to a significant improvement of the self-image. Being obese in itself may have an effect on negative affect, body dissatisfaction, self steem and eating behaviour [35]. A change in the situation would then partly affect changes in self control and this would be related to eating behavior and body dissatisfaction, which in turn would further affect the weight loss. On the other hand surgical intervention (gastric banding, vertical banded gastroplasty or gastric by-pass) affects feeling of fullness and satiety after meals would affect the weight loss too. We can speculate that the intervention modifies behavior in such a way that the patients improve the self-control and can reduce their impulsivity and self-image. The whole of the process is summarized in Figure 2.
How stable are these benefits? Considering that these patients are obese for more than 20 years on average, one year followup period may be too short. Future research will address longerterm effects of drastic weight reduction after surgery in eating behavior, body dissatisfaction, self steem, anxiety and depressive symptoms.
Conclusion
Morbid obesity is a risk poblation, which needs an evaluation, diagnosis and in psychiatric treatment in most cases. Bariatric Surgery promotes weight loss and an increase of satiety and self steem due to a subjective feeling of self control on the food intake and the improvement of the satisfaction with the own body.
References
- American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (4thedn.)Washington, DC.
- Pi-Sunyer FX: NHLBI Obesity Education Initiative Expert panel on the identification (1998), a valuation, and treatment of overweight and obesity in adults-the evidence report. Obesity Research; 6 2): S 51-209.
- Wolf AM, Kortner B, Kuhlmann HW (2001) Results of bariatric surgery. Int J ObesRelatMetabDisord 2 Suppl 1: S113-114.
- deZwaan M (2001) Binge eating disorder and obesity. Int J ObesRelatMetabDisord 25 Suppl 1: S51-55.
- Specker S, de Zwaan M, Raymond N, Mitchell J (1994) Psychopathology in subgroups of obese women with and without binge eating disorder. Compr Psychiatry 35: 185-190.
- Wadden T A, Foster G D, Letizia K A, Wilk J E (1993) Metabolic, anthropometric, and psychosocial characteristics of obese binge eaters. International Journal of Eating Disorders; 14: 17-25
- Yanovski SZ, Nelson JE, Dubbert BK, Spitzer RL (1993) Association of binge eating disorder and psychiatric comorbidity in obese subjects. Am J Psychiatry 150: 1472-1479.
- Black DW, Goldstein RB, Mason EE (1992) Prevalence of mental disorder in 88 morbidly obese bariatric clinic patients. Am J Psychiatry 149: 227-234.
- Goldsmith S J, Anger-friedfeld K, Beren S, Boeck M, Aronne L (1992) Psychiatric illness in patients presenting for obesity treatment. Int J Eat Dis; 12: 63-71
- Sarwer DB, Wadden TA, Foster GD (1998) Assessment of body image dissatisfaction in obese women: specificity, severity, and clinical significance. J Consult ClinPsychol 66: 651-654.
- Nieman DC, Custer WF, Butterworth DE, Utter AC, Henson DA (2000) Psychological response to exercise training and/or energy restriction in obese women. J Psychosom Res 48: 23-29.
- Rydén A, Sullivan M, Torgerson JS, Karlsson J, Lindroos AK, et al. (2004) A comparative controlled study of personality in severe obesity: a 2-y follow-up after intervention. Int J ObesRelatMetabDisord 28: 1485-1493.
- O'Neil PM, Jarrell MP (1992) Psychological aspects of obesity and very-low-calorie diets. Am J ClinNutr 56: S 185-189.
- Fitzgibbon ML, Stolley MR, Kirschenbaum DS (1993) obese people who seek treatment has different characteristics than those who do not seek treatment. Health Psychol 12: 342-345.
- Karlsson J, Sjoström L, Sullivan M. Swedish (1998)Obese subjects (sos)-an interevention study of obesity. Two year follow-up of health-related quality of life (HRQL) and eating behavior after weight reduction surgery in severe obesity.Int J ObesRelatMetabDisord; 22: 113-126
- Rydén A, Karlsson J, Persson LO, Sjöström L, Taft C, et al. (2001) Obesity-related coping and distress and relationship to treatment preference. Br J ClinPsychol 40: 177-188.
- Higgs ML, Wade T, Cescato M, Atchison M, Slavotinek A, et al. (1997) Differences between treatment seekers in an obese population: medical intervention vs. dietary restriction. J Behav Med 20: 391-405.
- Collins J, Beumont P, Touyz S, Gras J, Thompson B, Philips T. Variability in body shape perception in anorexic, bulimic, obese and control participants. International Journal of Eating Disorders 1987; 6: 633-638
- O'Brien KM, LeBow MD (2007) Reducing maladaptive weight management practices: developing a psychoeducational intervention program. Eat Behav 8: 195-210.
- Valtolina GG (1998) Body-size estimation by obese subjects. Percept Mot Skills 86: 1363-1374.
- Foster GD, Wadden TA, Vogt RA (1997) Body image in obese women before, during, and after weight loss treatment. Health Psychol 16: 226-229.
- Sisson BA, Franco SM, Carlin WM, Mitchell CK (1997) Body fat analysis and perception of body image. ClinPediatr (Phila) 36: 415-418.
- Leonhard ML, Barry NJ (1998) Body image and obesity: effects of gender and weight on perceptual measures of body image. Addict Behav 23: 31-34.
- Bardone-Cone AM (2007) Self-oriented and socially prescribed perfectionism dimensions and their associations with disordered eating. See comment in PubMed Commons below Behav Res Ther 45: 1977-1986.
- Henderson M, Freeman C P (1987) A self-rating scale for bulimia. The BITE. Br J Psychiatry; 150: 18-24.
- Beck A T, Ward C H, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961; 4: 561-571
- HAMILTON M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32: 50-55.
- Iqbal S, Ahmad R, Ayub N (2013) Self-esteem: a comparative study of adolescents from mainstream and minority religious groups in Pakistan. J Immigr Minor Health 15: 49-56.
- World Health Organization ICD-10.Mental Disorders. Madrid: Meditor, 1992
- Peltonen M1, Lindroos AK, Torgerson JS (2003) Musculoskeletal pain in the obese: a comparison with a general population and long-term changes after conventional and surgical obesity treatment. Pain 104: 549-557.
- Dhabuwala A1, Cannan RJ, Stubbs RS (2000) Improvement in co-morbidities following weight loss from gastric bypass surgery. ObesSurg 10: 428-435.
- Dixon JB1, Chapman L, O'Brien P (1999) Marked improvement in asthma after Lap-Band surgery for morbid obesity.ObesSurg 9: 385-389.
- Karasson K, Lindroos A, Stenlöf K, Sjöström L (2000) Relief of cardiorespiratory symptoms and increased physical activity after surgically induced weight loss: resluts from the Swedish Obese Subjects Study. Arch Internal Medicine; 160: 1797-1802
- Sorbara M1, Geliebter A (2002) Body image disturbance in obese outpatients before and after weight loss in relation to race, gender, binge eating, and age of onset of obesity. Int J Eat Disord 31: 416-423.
- Tice DM1, Bratslavsky E, Baumeister RF (2001) Emotional distress regulation takes precedence over impulse control: if you feel bad, do it! J PersSocPsychol 80: 53-67.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences